 Credit: MedicalGraphics.de, license CC BY-ND 4.0 Credit: MedicalGraphics.de, license CC BY-ND 4.0 Last year's flu season was a nasty one and this year's is just getting started. In my emergency department, we've begun to see a trickle of cases that is almost certain to herald an incoming surge. So brace yourselves, winter is coming. If you're experiencing flu symptoms (fever, chills, cough, sore throat, body aches, malaise, headache, vomiting and/or diarrhea), supportive care and time are unfortunately the only true avenues for relief (more on this later). Hopefully, you have an ample supply of Tylenol, tea, ginger ale and chicken soup. For the rest of you - flu vaccinated or just lucky - I want to set the record straight on some common flu misconceptions. In a social media post last flu season, my colleague Dr. Kim Sue (Massachusetts General Hospital, Internal Medicine) jokingly captured the frustration we feel as providers:
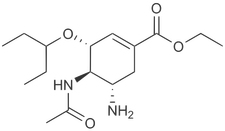
For providers, it often feels as though we are repeating ourselves year after year, answering the same questions and trying to quash the same misinformation. As a physician, I respect patient's autonomy to choose whether or not to get the flu vaccine each year. But what is equally important to me is that they make this choice based on sound information and also realize that this choice affects others in a meaningful way, including some of the most vulnerable among us. 1. I have the flu. As it turns out, not all illnesses that make you feel terrible are the flu. There are many potential causes of why we inevitably find ourselves under 5 blankets with a box of tissues, a mug of tea, the entire contents of our medicine cabinet and a long Netflix queue at least once every winter. These include rhinovirus (the common cold), coronavirus, respiratory syncytial virus (RSV), adenovirus, and parainfluenza among others. Less commonly, this same set of symptoms can also be a harbinger of other more ominous diagnoses such as meningitis or appendicitis. If you're ill enough to come to the hospital, we can run a pretty accurate PCR swab to confirm a case of influenza, but this ends up happening in a minority of cases. If you are feeling better within 1-2 days and you don't spike a true fever (>101.4˚ F), it probably wasn't the flu. 2. The flu shot doesn't work. The effectiveness of flu vaccination over the last several years has varied from 19-60%. This reality becomes easily warped into the myth that the shot doesn’t work at all. The truth is that the flu is a virus with numerous strains and a high rate of mutations which makes vaccine design a tricky business. Somewhere off in a lab each year, very smart people are thoughtfully making an educated estimate of the impending flu strains, several months in advance. And it simply is not possible to do this with 100% accuracy. By the time the vaccine has been manufactured and disseminated we can only wait and see how effective it will be for a given season. So yes, it is possible, as some patients will tell me that “I got the flu shot last year but I still got the flu". But that doesn’t negate the other truth that it saved lives, decreased illness and hospitalization and protected unvaccinated patients via partial herd immunity.
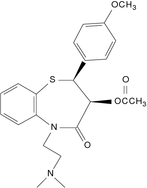
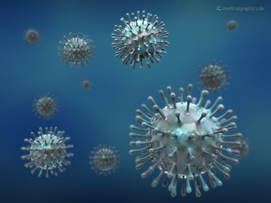
3. The flu shot gave me the flu. Typically, patients receive a trivalent or quadrivalent (3 or 4-strain) flu vaccination which can be grown via egg-culture, cell-culture or recombinant techniques or, less commonly, a live-attenuated intranasal vaccine. The bottom line is that all forms of the vaccine contain inactivated virus (traditional), weakened virus (intranasal) or simply parts of the flu virus (recombinant), none of which is capable of actually giving you the flu. Yes, you can get 1-2 days of malaise, fatigue, low grade fever and muscle aches after getting the vaccine, which is part of your body's normal immune response. Overall, the vaccine is well-tolerated and serious adverse events are very rare (much rarer than serious complications of the flu). Those couple of days of feeling run down are nothing compared to 3-7 days of debilitating symptoms with up to 2 weeks total recovery time for uncomplicated flu cases. 4. There's a cure for the flu. Yes, there is an antiviral medication out there that has some degree of activity against the flu virus. It’s called olsetamivir, but more commonly recognized by its trade name Tamiflu (the other FDA-approved antiviral is zanamivir or Relenza). It is true that it does something and the CDC does recommend that physicians “consider” administering it to flu patients in general and give it to high-risk patients. Overall, the available evidence* around Tamiflu, which was largely funded by industry, suggests that when given early in the flu course (in the initial 24-48 hours) that tamiflu decreases the duration of symptoms by less than one day. And it is not without risk of side effects, including increased incidence of confusion and psychiatric events, headache and nausea/vomiting. Turns out that there is an effective treatment that cuts flu symptoms to zero days! The flu shot! No, it’s not perfect but it’s quite a bit more perfect than Tamiflu. Of note, there is also a new, single-dose flu medication, called baloxavir (Xofluza) that was just approved by the FDA this October. The new drug was approved based on two clinical trials which showed a faster recovery time versus placebo, specifically about 23-28 hours. It isn't clearly better than Tamiflu, but the jury is still out on how it will perform in the general population. *Despite being FDA approved in 1999, it wasn't until 2014 that all clinical trial data was made fully available. For much of this period, despite significant national spending on Tamiflu, much of the data remained unpublished or selectively published by Roche Pharmaceuticals.
5. It's just the flu. Although the exact number of flu related fatalities is difficult to calculate, the CDC estimates that during the period from 2010 to 2015, annual flu-related deaths ranged from 12,000 to 56,000. Last year, it was over 80,000! An estimated 90 percent of deaths occurred in patients over 65 years old. Many of these patients died of complications of the flu, such as pneumonia, and had other co-morbid conditions that put them at higher risk. Young children, older adults (>65), pregnant women and those with asthma, COPD, heart disease and other conditions have a higher mortality risk. Yet each flu season, there are also fatalities among otherwise healthy children and adults. Also important to realize is that it may be 'just the flu' for most healthy patients, but it can also affect more vulnerable populations. The flu vaccinated patient has a decreased chance of contracting the flu (though non-zero) and if they never get sick then they never expose others. The non-vaccinated patient who does get sick continues to spread the flu virus potentially to the elderly, small children, asthmatics and other groups in which flu mortality is higher. I will never tire of giving a (educational) rant on the topic of vaccination and public health. I hope that in some small way this post can help fend off the onslaught of misinformation that troubles the internet and help contribute to reasoned discourse and scientific understanding on this topic. Feel better, America!
2 Comments
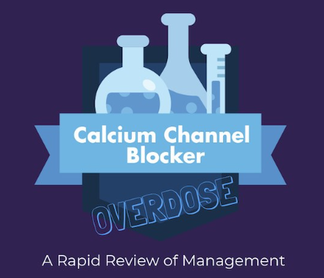
Thanks so much to all my friends and colleagues for voting for my submission to the 2018 Essentials of EM - Academic Life in EM Visual Design Competition. Congratulations to the winners, Dr. Liz Fierro and Dr. Natasha Li from Loma Linda University Health! While my entry was not selected for the grand prize, I was happy to see that it garnered the most views of all the submissions (over 6,000 as of this post). I'm very grateful for the exposure and all the supportive feedback from my EM colleagues.
I am very excited to announce that I have been selected as a semifinalist for the 2018 Academic Life in EM - Essentials of EM Visual Design Competition! 4 semifinalists were selected from submissions in various topics in emergency medicine. My submission was inspired by my recent blog post (see below) and is an infographic on management of calcium-channel blocker overdoses. The winner of the competition is selected for an EM Education Mini-Fellowship and is awarded travel to this year’s EEM Conference in Las Vegas in May 2018 where they support multiple aspects of the conference. VOTE HERE I would greatly appreciate your support! Voting is open to the public until Saturday, January 27 at 8pm. Please feel free to share! Recently, I took care of my first patient with a major calcium channel blocker (CCB) overdose. He was a middle aged man with unknown past medical history who had reportedly taken 20 tablets of diltiazem 120mg ER in a suicide attempt. Initial blood pressure in the field was 60/32, heart rate 30-40s. Knowing on an abstract level how sick these patients can get is one thing. Seeing it firsthand is something else entirely. Here are some lessons learned from a harrowing toxicological encounter.
Fortunately, this patient did well and ultimately did not need any 'end-of-the-line' therapies. This was a challenging yet valuable first brush with one of the sickest of all types of overdose patients. Like all difficult cases in the ED, teamwork and good communication were the bedrock of successfully managing the overdose. In the emergency department, we deal with a large volume of sick patients. Not only are many acutely ill, but they are often undifferentiated. Our daily lives include encounters with sepsis, STEMI, and shock and no shortage of other surprises. As a result, we develop a certain level of comfort with these high-stress situations.
Yet there are some encounters that move beyond even the daily ebb and flow of high acuity. These are the scenarios that make us break out in a cold sweat as the CMED call comes in. The ones that can form a knot in our stomachs even days or years later. Every clinician has cases like these that are seared into their memory, cases that help us grow as doctors. We sometimes refer to such patients as 'sick as stink' (SAS) - or even use a slightly more colorful version of the phrase. Though couched in the typical irreverence of the ED, this reference is not used in a derogatory manner. In fact, the expression is one of humility for the ways in which medicine can always continue to surprise and challenge us. It communicates a necessity for vigilance to our colleagues. It is an admission of how much a case affects us. These are the patients whose faces we can conjure effortlessly, who will become a symbol of what we learned, the unforgettable cases. SAS will be a recurring column on this site, a collection of my most memorable cases (de-identified as always). They will be mainly educational (rather than esoteric), meant to consolidate and share what I learned from these high stress encounters. I hope you enjoy the first installment! SAS - Episode 1 -J |
AuthorJoshua Feblowitz, MD, MS, is currently a PGY4 resident in the BWH/MGH Harvard-Affiliated Emergency Medicine Residency (HAEMR) Program and a freelance science writer. Archives
March 2019
Categories
All
|
||||||||||||