Thanks so much to all my friends and colleagues for voting for my submission to the 2018 Essentials of EM - Academic Life in EM Visual Design Competition. Congratulations to the winners, Dr. Liz Fierro and Dr. Natasha Li from Loma Linda University Health! While my entry was not selected for the grand prize, I was happy to see that it garnered the most views of all the submissions (over 6,000 as of this post). I'm very grateful for the exposure and all the supportive feedback from my EM colleagues.
0 Comments
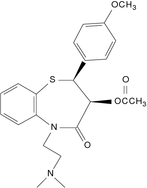
I am very excited to announce that I have been selected as a semifinalist for the 2018 Academic Life in EM - Essentials of EM Visual Design Competition! 4 semifinalists were selected from submissions in various topics in emergency medicine. My submission was inspired by my recent blog post (see below) and is an infographic on management of calcium-channel blocker overdoses. The winner of the competition is selected for an EM Education Mini-Fellowship and is awarded travel to this year’s EEM Conference in Las Vegas in May 2018 where they support multiple aspects of the conference. VOTE HERE I would greatly appreciate your support! Voting is open to the public until Saturday, January 27 at 8pm. Please feel free to share! Recently, I took care of my first patient with a major calcium channel blocker (CCB) overdose. He was a middle aged man with unknown past medical history who had reportedly taken 20 tablets of diltiazem 120mg ER in a suicide attempt. Initial blood pressure in the field was 60/32, heart rate 30-40s. Knowing on an abstract level how sick these patients can get is one thing. Seeing it firsthand is something else entirely. Here are some lessons learned from a harrowing toxicological encounter.
Fortunately, this patient did well and ultimately did not need any 'end-of-the-line' therapies. This was a challenging yet valuable first brush with one of the sickest of all types of overdose patients. Like all difficult cases in the ED, teamwork and good communication were the bedrock of successfully managing the overdose. In the emergency department, we deal with a large volume of sick patients. Not only are many acutely ill, but they are often undifferentiated. Our daily lives include encounters with sepsis, STEMI, and shock and no shortage of other surprises. As a result, we develop a certain level of comfort with these high-stress situations.
Yet there are some encounters that move beyond even the daily ebb and flow of high acuity. These are the scenarios that make us break out in a cold sweat as the CMED call comes in. The ones that can form a knot in our stomachs even days or years later. Every clinician has cases like these that are seared into their memory, cases that help us grow as doctors. We sometimes refer to such patients as 'sick as stink' (SAS) - or even use a slightly more colorful version of the phrase. Though couched in the typical irreverence of the ED, this reference is not used in a derogatory manner. In fact, the expression is one of humility for the ways in which medicine can always continue to surprise and challenge us. It communicates a necessity for vigilance to our colleagues. It is an admission of how much a case affects us. These are the patients whose faces we can conjure effortlessly, who will become a symbol of what we learned, the unforgettable cases. SAS will be a recurring column on this site, a collection of my most memorable cases (de-identified as always). They will be mainly educational (rather than esoteric), meant to consolidate and share what I learned from these high stress encounters. I hope you enjoy the first installment! SAS - Episode 1 -J |
AuthorJoshua Feblowitz, MD, MS, is currently a PGY4 resident in the BWH/MGH Harvard-Affiliated Emergency Medicine Residency (HAEMR) Program and a freelance science writer. Archives
March 2019
Categories
All
|
||||||